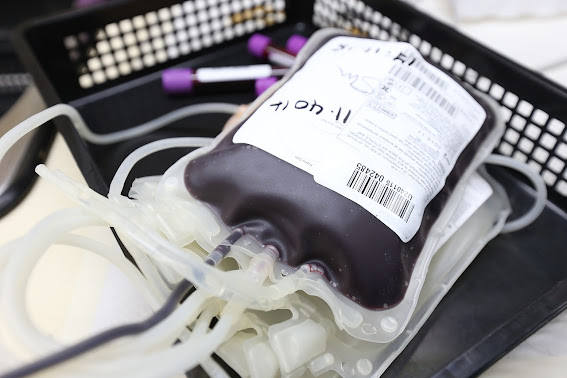
Blood transfusions save countless lives every day, from accident victims to cancer patients undergoing chemotherapy. Yet, despite the critical importance of maintaining a steady blood supply, blood banks across the world frequently report shortages. Why is this a chronic challenge? The reasons span societal patterns, seasonal variations, and industry-specific complications.
The Summer Slump: College Closures and Vacationing Donors
For many, summer evokes images of sun-soaked beaches, barbecues, and long-awaited vacations. However, for blood banks, summer often sounds an alarm. A significant portion of blood donations comes from college and university blood drives. These institutions, with their dense populations of young and often healthy individuals, can be gold mines for blood donations. But once summer starts, campuses empty out, leaving blood banks with a gaping hole in their usual donation numbers.
Furthermore, summer isn’t just a time for students to take a break; it’s the peak travel season. Families, individuals, and even regular donors jet off to vacations, making it less likely for them to donate. While a week-long trip might seem inconsequential, the cumulative effect of many potential donors being away can severely impact blood supplies.
Holidays: A Double-Edged Sword
Holidays, much like summers, are times of joy and relaxation for most. But for blood banks, they can be periods of dread. Holiday weekends see a surge in travel, making potential donors less accessible. Moreover, during festive times, individuals are engrossed in preparations, celebrations, and family gatherings, often placing blood donation low on their priority list. This results in a drop in the blood supply, just when more accidents typically occur due to increased travel, leading to a greater demand for transfusions.
Staffing Struggles in the Blood Donation Realm
Behind every blood donation, there’s an army of professionals ensuring the process runs smoothly. Phlebotomists, the trained professionals who draw blood, are the frontline soldiers in this battle against shortages. Their expertise ensures that blood is drawn safely, efficiently, and with minimal discomfort to the donor.
However, like many specialized professions, there’s a shortage of skilled phlebotomists. The reasons are manifold. Phlebotomy, despite its importance, may not offer competitive remuneration in all regions or institutions. The job, being hands-on and requiring impeccable precision, can be high-pressure. Mistakes are not an option, leading to a steep learning curve and rigorous training requirements.
Then there are the couriers, the vital links that ensure donated blood reaches its destination promptly. These individuals often work irregular hours, handling delicate packages that can mean life or death for someone. The demand for timely transportation of blood can be especially high during emergencies or natural disasters.
Drive workers, the people who set up and manage the infrastructure for blood drives, also face unique challenges. Organizing a drive requires meticulous planning, coordination with multiple agencies, and the ability to manage large groups of donors. Finding individuals skilled in such tasks, willing to work on a schedule dictated by the community’s needs, can be daunting.
Operational Hiccups and Challenges
Maintaining a consistent blood supply isn't just about getting donors in the door. It's a complex ballet of logistics, where blood collected needs to be tested, processed, stored, and then dispatched as required. Each of these stages requires specialized staff, equipment, and facilities. Even minor disruptions, be it equipment malfunctions or delays in transportation, can cause bottlenecks. With blood having a limited shelf life – 42 days for red blood cells and just five days for platelets – these delays can result in wastage, further exacerbating shortages.
Public Perceptions and Myths
Misconceptions surrounding blood donations can also play a role in shortages. Fears about pain, side effects, or contracting diseases deter potential donors. While awareness campaigns are working to combat these myths, they persist in sections of the community, creating barriers to donation.
Pandemics and Health Crises
Global health crises, such as the COVID-19 pandemic, pose unprecedented challenges for blood banks. The fear of getting infected deters many potential donors from visiting donation centers. Moreover, lockdowns and social distancing measures further limit the ability to conduct large-scale donation drives. During the initial stages of the pandemic, many blood drives were canceled, causing an immediate and concerning drop in available blood supplies.
The Financial Dynamics
Blood donation, at its heart, is a philanthropic act, but the operations surrounding it are undoubtedly bound by financial constraints. Blood banks have to balance between operational costs, testing, storage, and transportation. Profit margins can be slim, especially for non-profit blood centers. The economics becomes even more challenging when there's a need for rare blood types or specialized blood products, which might cost more to process but are essential for specific patient populations.
Generational Shifts in Attitudes
While it's a broad generalization to say newer generations don’t recognize the importance of donating blood, there has been a noted shift in outreach methods needed to engage them. Traditional awareness campaigns might not resonate as much with younger generations, necessitating a shift to digital platforms, influencers, and other modern outreach strategies. If these shifts aren't made promptly or effectively, it can lead to decreased engagement from younger potential donors.
Educational Gaps
Over the years, there has been a fluctuation in emphasis on community service and civic duties in educational curriculums. While some schools and colleges have robust programs encouraging blood donation, others might lack such initiatives. A consistent, nationwide (or even global) emphasis on the importance of blood donation in educational settings could help instill the habit in individuals from a young age.
Commercialization and Profit Motives
Some blood banks operate on a for-profit model, leading to concerns about the commercialization of what many see as a purely altruistic act. This commercial angle can sometimes deter potential donors who might feel uneasy about their donation becoming a commercial product. It's a delicate balance for these institutions to maintain operational efficiency while ensuring the trust of the donor community.
Regional Disasters and Traumas Impacting Blood Supplies
Every region, whether it's due to its geographical location, climate, or other factors, is vulnerable to specific types of disasters. For instance, coastal areas might face hurricanes, while tectonically active zones could be at risk of earthquakes. When these disasters strike, the medical needs of the affected populace surge dramatically, including a sudden increase in demand for blood.
Natural disasters often result in injuries that require surgical interventions, thereby increasing the demand for blood products. Similarly, large-scale accidents or mass trauma incidents, like major vehicle pile-ups or industrial accidents, can exert sudden pressure on available blood supplies.
Concurrently, these disasters can disrupt regular blood donation activities. Blood banks in the affected areas might be damaged, or transportation routes could be blocked, preventing the timely arrival of much-needed blood from other regions. Also, regular donors might be affected by the disaster themselves, making them temporarily unavailable to contribute.
Moreover, even if a region isn't directly affected by a disaster, it might be called upon to support a neighboring area that is. This can strain local supplies, especially if there's already an existing shortage.
Understanding the dual challenge posed by increased demand and potential disruptions during disasters underscores the need for robust contingency plans. Blood banks, in collaboration with local and national agencies, must be prepared to rapidly scale up their operations and ensure that they can meet the sudden surge in demand while also navigating the logistical challenges posed by the disaster.
What now?
The persistent problem of blood shortages, at its core, is a multi-faceted challenge. It intertwines with societal behaviors, professional shortages, operational challenges, and public perceptions. Addressing it requires not just rallying more donors but also creating robust systems that can efficiently handle donations, fostering professional growth in the industry, and constantly battling misconceptions with information. As our understanding of these intricacies grows, so does our hope for a future where blood shortages become a relic of the past.