 |
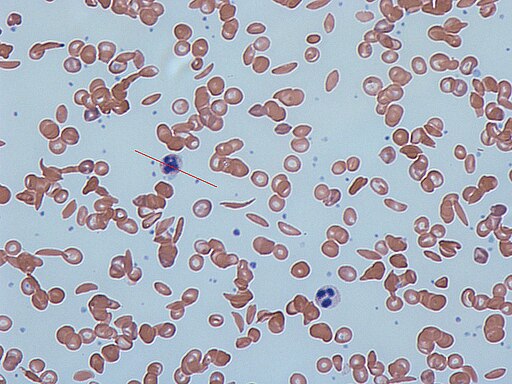
| Sickled Cells on a blood smear |
What is Sickle Cell Disease
Sickle cell disease (SCD) is a genetic blood disorder that affects millions of people worldwide. It causes red blood cells to become sickle-shaped and stiff, which can block blood flow to various organs and tissues, leading to severe pain, organ damage, and even death.
Sickle cell disease is most common in people of African descent, but it also affects people of Hispanic, Middle Eastern, and Mediterranean descent. There is no cure for sickle cell disease, but treatments can help manage symptoms and reduce complications. Transfusion therapy can help manage the complications of SCD, but it also poses risks, and its use needs to be carefully considered.
Understanding Sickle Cell Disease and its Complications
SCD is caused by a mutation in the HBB gene that affects the production of hemoglobin, the protein that carries oxygen in red blood cells. Instead of the normal round shape, the hemoglobin molecules in people with SCD form stiff, sickle-shaped structures. These sickle cells can get stuck in small blood vessels, leading to inflammation, tissue damage, and severe pain, particularly in the bones, chest, and abdomen. Repeated episodes of pain can lead to organ damage and increase the risk of infections, stroke, and other complications.
Transfusion therapy for Sickle Cell Disease
Transfusion therapy can help manage the complications of SCD by providing healthy red blood cells that can improve oxygen delivery and prevent sickling. The goals of transfusion therapy for SCD include reducing the frequency and severity of pain episodes, preventing or treating strokes, and reducing the risk of acute chest syndrome, a potentially life-threatening complication that can occur when sickle cells block blood vessels in the lungs.
However, transfusion therapy also carries risks, including the development of alloantibodies, iron overload, and infections. Alloantibodies are antibodies produced by the immune system in response to foreign red blood cells from donors. In SCD patients who receive frequent transfusions, alloantibodies can accumulate and make it difficult to find compatible blood for transfusion. Iron overload can occur when the body absorbs too much iron from the transfused blood, leading to organ damage, particularly in the heart and liver. Finally, chronic transfusions can increase the risk of infections and other transfusion related sequela.
Transfusion needs in SCD patients
The decision to transfuse SCD patients depends on various factors, including the severity of their symptoms, the presence of complications, and their overall health. In general, SCD patients with a hemoglobin level below 6 g/dL or with evidence of tissue damage or organ dysfunction may benefit from transfusion therapy. However, transfusions should be used judiciously and tailored to the individual patient's needs to minimize the risks of complications.
Rh and Kell Antigen Screening
SCD patients require Rh and Kell antigen screening before receiving transfusions. Rh and Kell antigens are present on the surface of red blood cells and can cause alloimmunization, which is the production of antibodies against these antigens. As many SCD patient's are chronically transfused, they are at a higher risk of developing alloantibodies, the most common being antibodies in the Rh system such as D,C, or E and also Kell. If SCD patients with Rh or Kell antibodies receive blood containing these antigens, their immune system will attack the donor red blood cells, leading to a severe transfusion reaction. Therefore, SCD patients require Rh and Kell antigen-negative blood to avoid these complications.
HgbS Negative Blood
SCD patients also require blood that is tested to be HgbS negative. HgbS is the abnormal hemoglobin that causes sickling of red blood cells in SCD patients. If SCD patients receive blood containing HgbS, their red blood cells will still sickle, and they will not benefit from the transfusion. Therefore, SCD patients require blood that is tested to be HgbS negative.
Transfusions and Sickle Cell Trait
Individuals with sickle cell trait typically do not require blood transfusions. Sickle cell trait is a genetic condition where a person inherits one normal hemoglobin gene and one abnormal hemoglobin gene. While individuals with sickle cell trait may have some symptoms related to the abnormal hemoglobin gene, these symptoms are usually mild and do not require blood transfusions.