What is Bombay phenotype?
The Bombay phenotype is a rare blood type that occurs when an individual has inherited two copies of a recessive gene that affects the production of certain antigens on the surface of red blood cells. Specifically, individuals with Bombay phenotype do not produce the H antigen, which is the precursor to the A and B antigens that determine the ABO blood type system. As a result, people with Bombay phenotype have blood that appears to be type O, even though they may have genes for type A or B blood.
How does Bombay phenotype affect transfusions?
Because people with Bombay phenotype lack the H antigen, their blood can be incompatible with blood from other ABO blood types. This means that people with Bombay phenotype cannot receive blood from most other blood types, including type A, B, AB, and O. In fact, people with Bombay phenotype can only receive blood from other individuals with the same rare blood type.
For this reason, it is essential that individuals with Bombay phenotype are identified and properly tested before any blood transfusions. If someone with Bombay phenotype receives blood from an incompatible blood type, it can lead to a severe and potentially life-threatening reaction known as a transfusion reaction.
What steps can be taken to ensure safe transfusions for people with Bombay phenotype?
To ensure the safety of people with Bombay phenotype who require blood transfusions, it is crucial to identify individuals with this rare blood type early on. This can be done through blood typing tests, which can determine whether or not someone has the H antigen.
Once someone with Bombay phenotype has been identified, steps can be taken to ensure that they receive compatible blood during transfusions. This typically involves identifying other individuals with the same rare blood type and maintaining a supply of their blood for use in transfusions. Blood banks and hospitals often work together to create networks of donors with rare blood types, including Bombay phenotype, to ensure that there is always a supply of compatible blood available.
In addition to proper identification and blood banking, it is also important to monitor people with Bombay phenotype closely during and after blood transfusions. This can help to identify any potential complications or adverse reactions early on and ensure that prompt treatment is provided if necessary.
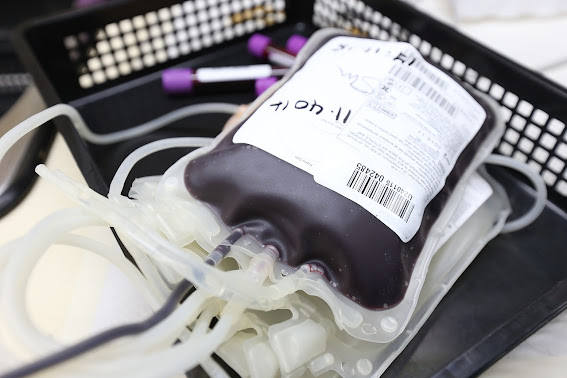
Frozen Blood
Blood for people with Bombay phenotype can be frozen and stored for future use, and one of the most common methods of blood preservation is glycerolization.
Glycerolization is a process in which red blood cells are mixed with a solution of glycerol and other chemicals before freezing. This solution helps to protect the cells from damage during the freezing and thawing process and allows the blood to be stored for longer periods of time.
During glycerolization, the red blood cells are mixed with a solution containing glycerol, a sugar called trehalose, and other chemicals that help to stabilize the cells. The cells are then slowly cooled to a temperature below freezing, typically around -80°C. Once the cells are frozen, they can be stored for several years, if necessary, without significant loss of quality.
When the blood is needed for transfusion, the frozen blood is thawed slowly and carefully, and the glycerol and other chemicals are removed. The red blood cells can then be transfused into the patient as needed.
Glycerolization is a common method of blood preservation for people with rare blood types like Bombay phenotype because it allows compatible blood to be stored for longer periods of time, which can be especially important in emergency situations or when a suitable donor is not immediately available.
Autologous Donation
People with Bombay phenotype can donate their own blood for autologous transfusions. In fact, autologous blood donation can be a valuable strategy for people with rare blood types like Bombay phenotype to ensure that they have access to compatible blood when needed.
Autologous blood donation involves collecting and storing a person's own blood for future transfusion. The process usually involves donating blood several weeks or months before it is needed, and the blood is tested and processed to ensure that it is safe and compatible with the person's own blood type.
Because people with Bombay phenotype have a rare blood type that is not compatible with most other blood types, autologous blood donation can be a useful strategy for ensuring that they have access to compatible blood when needed. It can be particularly important in situations where there may be limited access to compatible blood, such as in remote or resource-limited settings.
It's important to note that the process of autologous blood donation and transfusion requires careful planning and coordination to ensure that the blood is collected, processed, and stored properly, and that it is used before it reaches its expiration date.