Transfusing Blood Products, especially with today's modern medical advancements, is a very safe and effective procedure. Blood Centers and Transfusion Center Blood Banks aim to provide the smoothest and safest transfusion possible. However, like with any procedure, there are risks involved.
What Is A Transfusion Reaction?
A transfusion reaction is simply a body's adverse reactions to a blood component or its constituents. Reactions can range from mild, to severe, to even death. It is imperative that the patient's vital signs and over health be taken in account prior to transfusion and must also be closely monitored during and after transfusion. It is common to measure pre, during, and post-vital signs such as body temperature, heart rate, blood pressure, O2 saturation, and respiratory rate. A drastic change in these during or after transfusion can signal a potential transfusion reaction. A patient may present with more obvious and visual signs of a transfusion reaction as well.
If signs of a transfusion reaction are present, the transfusion should be stopped immediately. Typically, best practices dictate that the IV stays open with normal saline (0.9% NS). Follow your own hospital guidelines. The unit of Blood and the patient tag or label on the blood should be checked for clerical errors. Was the correct blood type given? Is this the correct patient? Any discrepancies must be called to the Blood Bank department immediately.
Alert the physician so that a Transfusion Reaction workup can be performed by the Blood Bank. This typically involves drawing a post-transfusion specimen and retrieving a urine. The Blood Bank will check to ensure there are no errors in wrong historic Blood Type, perform a Direct Antiglobulin Test to ensure there are no antibodies coating the patient's cells, perform their own clerical check on the unit, ensure all Blood Bank file transfusion guidelines were followed, as well as visually checking the pre and post transfusion samples for hemolysis or icterus.
CLICK THE LINKS BELOW TO JUMP TO A REACTION TYPE
MILD ALLERGIC TRANSFUSION REACTION
Mild Allergic transfusion reactions are one of the most common type of transfusion reaction seen. It is generally not severe or life-threatening and may only amount to a nuisance for the patient. These types of reactions are more common in platelet transfusions than Red Blood Cells, likely due to the increased amount of plasma exposure, thus plasma protein exposure received. An allergic type reaction could be seen in up to 3% of all platelet transfusions. With Red Cells, it's typically less than 1%.
 |
| Designed by brgfx / Freepik |
bronchospasms (wheezing).
These reactions are generally caused by an immune system hypersensitivity towards certain plasma proteins in the donor unit. Although rare, it is even possible for common allergens to be transferred through the plasma to cause an allergic reaction in the recipient. For example, a donor with penicillin in their plasma could cause the recipient to have a reaction if they are allergic to the antibiotic. Food allergens have been implicated in this as well.
Often times, those known to have allergic transfusion reactions can and will be given an antihistamine, such as diphenhydramine (Benadryl) to mitigate the allergic effects of the transfusion. If symptoms remain mild, depending on your individual location's procedures, the transfusion can continue.
Allergic transfusion reactions have been cut nearly in HALF through the use of Platelet Additive Solution (PAS) technologies. PAS platelet units have roughly 65% of their plasma removed and replaced with an additive solution that helps keep the platelets alive and shelf stable. This reduction in plasma greatly reduces the exposure to donor plasma proteins limiting the amount of allergic reactions seen in transfusion.
ANAPHYLACTIC TRANSFUSION REACTION
FEBRILE NON-HEMOLYTIC TRANSFUSION REACTION
 |
| Designed by pikisuperstar / Freepik |
FNHTR are generally thought to arise as a result of cytokine release from white blood cells. Although most blood products in this day and age are leukoreduced, this process doesn't remove ALL white blood cells from a unit of blood. As a unit of platelets or red blood cells age, the remaining white blood cells in the unit may start to release cytokines as they themselves start to age and breakdown. Cytokines are a broad category of proteins that are involved in cell signaling and immune system modulation. Their presence generally leads to inflammation, which then leads to fever. Transfusion of fresher units may lower the incidence of FNHTRs.
Symptoms of a FNHTR can typically be relieved with acetaminophen/paracetamol.
ACUTE HEMOLYTIC TRANSFUSION REACTION
Acute Hemolytic Transfusion Reactions (AHTR) are a rare but serious transfusion reaction. It is most commonly associated with receiving ABO Blood Type incompatible blood in which the recipient's isoagglutinin antibodies attack the incompatible blood, causing the Red Cells to be destroyed. For example, an O positive patient who received an A positive Red Blood Cell unit by mistake could potentially have an Acute Hemolytic Transfusion reaction due to the fact that O positive patients have Anti-A and Anti-B isoagglutins in their plasma. This type of reaction is rare, but generally happens due to human error. Yet, nearly 50% of ABO incompatible transfusions will not amount to an AHTR. The reactions that do happen, have roughly a 5% fatality rate. The AABB (Association for the Advancement of Blood and Biotherapies) now requires that all accredited transfusion center Blood Banks have two separate Blood Type draws on file before they can receive type specific (Non type O) Red Blood Cells. This is to help eliminate pre-transfusion errors such as misdrawing or mislabeling a patient's specimen.
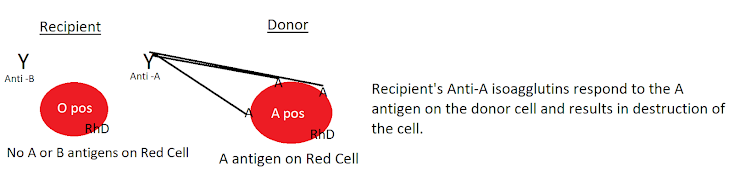 |
| Anti-A in the O positive recipient's plasma attacks the A antigen on the A pos Donor Blood causing an acute hemolytic transfusion reaction. |
AHTRs can also happen as a result of antibody/antigens mismatches outside of the ABO/Rh system. Kidd, Duffy, and Kell antigen systems have been implicated in some AHTRs. This is why it is extremely important for a transfusion center Blood Bank to identify any alloantibodies on a patient. Alloantibodies are antibodies that a patient has made to Red Cell antigen systems in which they lack through Red Cell exposure (such as through transfusion or pregnancy). For example, if a patient is Jk(a) negative and receives a Jk(a) positive unit, they may create an Anti-Jk(a). From then on, it is imperative they receive Jk(a) negative blood products, if they do not, they may have an AHTR.
An AHTR can be trigged by only a few milliliters of blood and symptoms typically begin during the transfusion or very shortly after receiving the product which is why an AHTR can also be referred to as an Immediate Hemolytic reaction.
AHTRs can present with symptoms similar to other type reactions such as fever, chills, abdominal pain, trouble breathing, hypotension, etc. Back pain and oliguria/anuria is possible as well. Patients will also present with hemoglobinuria (hemoglobin in the urine) and hematuria (blood in the urine) which is a hallmark for hemolytic reactions. Hemoglobin is the main protein comprising a Red Blood Cell. A hemolytic reaction results in the destruction of Red Blood Cells causing excess hemoglobin to enter the blood stream. The kidneys filter out the hemoglobin and process it into urine for removal from the body (this excess of hemoglobin can cause kidney damage/acute kidney injury as well. This will usually result in a red or more likely brown (tea-like) urine. More severe reactions can progress to shock and DIC (Disseminated Intravascular Coagulation). A consequence of red cell hemolysis, increased anemia can result as well.
There are specific lab tests that can help diagnose an AHTR. A urinalysis may show positive hemoglobin. A Direct Coombs test which looks for antibodies that are coating the Red Cell, may be positive. Plasma bilirubin may be elevated, and haptoglobin will be decreased. A CBC with differential may show red cell fragments. A patient's urine/plasma may also look hemolyzed (red or brown color to it).
DELAYED HEMOLYTIC TRANSFUSION REACTION
Delayed Hemolytic Transfusion reactions are similar to Acute Hemolytic Reactions. Unlike AHTRs, Delayed Hemolytic Transfusion Reactions (DHTRs) typically take days to weeks to show clinically and do not cause an immediate reaction. DHTRs typically result from a patient forming an antibody to an antigen outside of the ABO system. Remember, ABO blood type mismatches generally cause Acute Hemolytic reactions. DHTRs can occur when a patient comes in contact with blood that is positive for antigens they are negative for. Their immune system sees it as foreign and creates an antibody towards this antigen, remembering it for next time. This initial sensitization event may not spark a huge immune response.
Thus, when the patient has pre-transfusion testing performed, the antibody that was created may be circulating in such low levels that it is not detectable by typical Immunohematology methods. The transfusion center Blood Bank would then not be aware of this antibody and potentially provide blood that is antigen positive. This would then cause an "anamnestic response" in which the immune system reacts at a much greater rate then before. Days to weeks after the transfusion, enough antibodies are created to potentially cause a hemolytic reaction. Antibodies towards the Kidd antigen system (such as Jk(a) and Jk(b) are known for their ability to evade detection and cause subsequent reactions).
Symptoms are similar to that of an acute hemolytic response. Patients may have an increased plasma bilirubin (and appear jaundiced) and Lactate Dehydrogenase, decreased haptoglobin, increased in reticulocytes (immature Red Blood Cells), a positive Direct Antiglobulin test indicating antibodies are coating the Red Blood Cells, not having the correct response to Red Cells (i.e Hemoglobin and Hematocrit not increasing or even decreasing post-transfusion).
Patients with known antibodies must receive blood negative for these antigens to ensure events like this won't happen!
TRALI
This is because occasionally at some point during gestation or child-birth the mother may come in contact with blood from the baby and be exposed to HLA antigens that the mother may not have. This would cause the mother to create Anti-HLA antibodies. Many blood centers have procedures on how to handle this to mitigate the effects of TRALI.
TRALI causes hypothesis
TACO
SEPTIC TRANSFUSION REACTION
- During collection -- If the nurse or phlebotomist collecting the unit of blood does not practice proper aseptic technique. The site in which blood will be taken from should be cleaned with an alcohol wipe or iodine preparation, gloves should worn and hands should be cleaned, the disinfected area should not be touched again prior to collection, all tools should be free from contamination, etc.
- Donor bacteremia -- Although rare, it is possible that the donor themselves has bacteremia (bacteria in their blood) and may not be aware or event present with symptoms.
- Contaminated collection bags. Occasionally blood collection bags could have rips,tears,or holes that aren't noticed by the naked eye but are big enough for bacteria/fungi/etc. to enter and infect the product. It is also possible for bacteria to be on the outside of the bag, and enter the bag through imperfect aseptic technique.
- Contamination during processing of the units -- Units can potentially be contaminated during the processing of the unit into components. There are many procedures and equipment (such as a sterile welder) that help mitigate this issue.
Contamination at a transfusion center during product manipulation -- A transfusion center blood bank may inadvertently contaminate a product while manipulating a product, such as splitting a unit of platelets into a smaller unit for pediatric transfusion or pooling units of thawed cryoprecipitate together.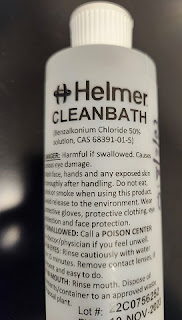
Benzalkonium Chloride solution for a
Plasma Thawer water
treatment to prevent microbial growth
Additionally, units of frozen plasma or cryoprecipitate can have their port openings contaminated either by simple handling or through the water contact in a Plasma Thawer. Many transfusion center blood banks opt to use a water bath cleaner to ensure bacterial/fungal growth does not happen in the water. The water is also flushed and new fresh water added at least once a week. Pseudomonas aeruginosa is commonly found in contaminated water baths.
Platelets that have been on the shelf for few days have a higher risk of contamination due to longer incubation time of a pathogen. Red Blood Cells can still cause septic reactions, especially if they have been sitting in the fridge for an extended period of time (multiple weeks), but refrigeration slows the growth and proliferation of any contaminating pathogen (except for certain bacteria such as Yersinia enterocolitica which prefer colder temperatures). Any contamination in a frozen product is generally from post-thaw activity, because the act of freezing the product post-collection is generally enough to kill the pathogens.