DNA and Genetic Information: At the heart of every cell in our body lies a nucleus (except mature red blood cells, which we'll delve into shortly). Within this nucleus is deoxyribonucleic acid (DNA), the molecule that contains our genetic code. This code acts as an instruction manual for our body – from determining our hair color and height to more complex processes like metabolism.
Blood Transfusions and Their Components: Blood transfusions aren't just about transferring red blood cells. Blood comprises several components: red blood cells, white blood cells (WBCs), platelets, and plasma. When a person receives a blood transfusion, depending on the requirement, they could receive any of these components. The most common transfusion, however, is the red blood cell transfusion.
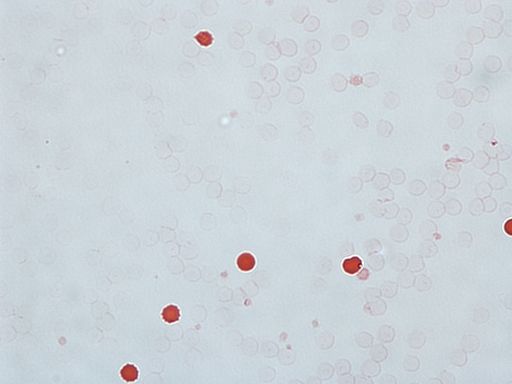
Mature Red Blood Cells and Their Lack of Nucleus: Red blood cells are unique. Unlike other cells in our body, mature RBCs do not have a nucleus. This absence is actually by design. RBCs are primarily responsible for transporting oxygen from the lungs to the rest of the body and carrying carbon dioxide from the body's tissues back to the lungs. To maximize space for the oxygen-binding molecule, hemoglobin, RBCs eject their nucleus as they mature. This means that mature RBCs do not possess DNA.
Given this, when a person receives a transfusion of mature red blood cells, they are not receiving any DNA from the donor in those RBCs.
Reticulocytes and Their Genetic Material: While mature RBCs lack a nucleus, their precursors, called reticulocytes, do contain a nucleus. Reticulocytes are immature RBCs, and as they mature into functional RBCs, they eventually lose their nucleus. In a typical blood transfusion, the vast majority of cells are mature RBCs. However, a small number of reticulocytes might also be present. While these reticulocytes contain DNA, their presence is minuscule in comparison to the total blood volume.
White Blood Cells and DNA Transfer: Unlike RBCs, white blood cells (WBCs) do have nuclei and, therefore, contain DNA. However, transfusions are usually filtered to reduce the number of WBCs due to concerns about potential immune reactions. So, the number of WBCs (and thus the amount of donor DNA) in transfused blood is minimal.
Does Donor DNA Integrate into Recipient Cells? Even if small amounts of donor DNA enter the recipient's bloodstream through transfused WBCs or reticulocytes, this DNA does not integrate into the recipient's cells or genetic code. Our DNA remains stable and unchanged. The donor DNA present in WBCs or reticulocytes would eventually be degraded and cleared from the recipient's body.
Implications and Misconceptions: There have been misconceptions and myths surrounding blood transfusions, especially in popular culture. Stories of individuals acquiring memories or traits of their donors are scientifically unfounded. A blood transfusion does not alter a person's genetic makeup or bestow them with the characteristics or memories of the donor.
COVID-19 vaccine: Conspiracy Theories floating around have also said that the vaccine can alter or change your DNA. Welllll no it doesn't. Nor does receiving blood products from a patient who received the coronavirus vaccine. And no... You can't request unvaccinated blood.
So, In essence, a blood transfusion does not change a recipient's DNA. While there may be trace amounts of donor DNA present in the transfused blood due to the minuscule number of reticulocytes or white blood cells, these do not integrate with the recipient's DNA. The primary purpose of a transfusion is to replenish the body's supply of essential blood components, especially red blood cells, to ensure the effective transport of oxygen throughout the body. Understanding the nuances of how transfusions work and their impact on the body is crucial in dispelling myths and emphasizing the life-saving potential of this medical procedure.