Platelet Rich Plasma Injections
Platelet-rich plasma (PRP) injections have been gaining attention in both the medical and sporting world. As transfusion medicine continues to evolve, PRP offers promising therapeutic applications for various conditions. Let's explore the science, benefits, and considerations surrounding PRP in transfusion medicine.
What is Platelet-Rich Plasma?
Platelet-rich plasma (PRP) is derived from the blood and stands out because of its high concentration of platelets, surpassing what's typically found in the bloodstream. To comprehend the significance of this, it's essential to recognize the roles platelets play.
Platelets: More than Just Clotting Agents
While platelets are popularly known for their role in clotting blood, they are biological treasure troves packed with proteins and molecules that are vital for tissue repair and regeneration. Some of these key components include:
Growth Factors: These are proteins that facilitate cellular growth, proliferation, and differentiation. In the context of injuries, they can accelerate tissue repair. For instance, the platelet-derived growth factor (PDGF) stimulates cell replication, and the vascular endothelial growth factor (VEGF) promotes the formation of new blood vessels, which is crucial for healing.
Cytokines: These are cell signaling molecules that facilitate communication and interaction between cells. They play a pivotal role in modulating the immune response and inflammation, two processes intricately linked with healing.
Adhesion Molecules: These help platelets stick to each other and to other cells, ensuring that they can effectively participate in the repair process.
Ethical Issues in Transfusion Medicine
Autonomy and Informed Consent
Informed consent is a cornerstone of ethical medical practice. Patients have the right to understand the benefits, risks, and alternatives before receiving a transfusion. However, the urgency of some situations may complicate this process.
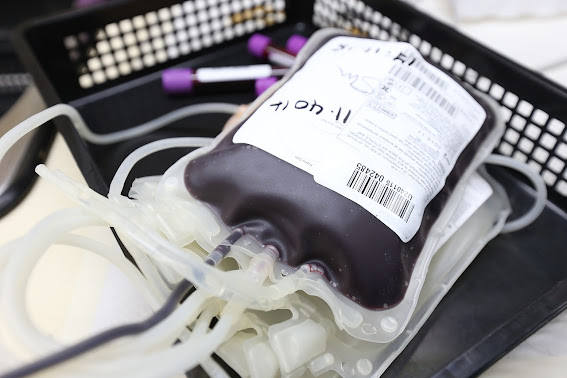
Whole Blood Transfusion
Why Use Whole Blood?
Whole blood transfusions reintroduce the practice of using unmodified, non-separated blood, essentially as it's drawn from the donor, albeit with certain standard treatments such as leukoreduction and pathogen reduction. It is generally only given as O positive or O negative and is tested to high low titers of ABO isoagglutinins to limit the possibility of an incompatibility reaction in a non type O patient.
Massive Hemorrhage Protocols: In situations of traumatic injuries or major surgeries resulting in rapid and significant blood loss, whole blood transfusions can be beneficial. The patient loses not just red cells but also platelets, clotting factors, and plasma. Whole blood provides all these elements in a balanced proportion.
Cryopoor Plasma (CPP)
Cryopoor plasma [CPP] (or cryosupernatant) is a component derived from blood, is a lesser-known product of blood separation. Understanding what it is, its uses, and the complexities surrounding its application and storage, can provide deeper insight into its critical role in transfusion medicine.
What is Cryopoor Plasma?
Plasma is the liquid component of blood, primarily composed of water, electrolytes, proteins, hormones, waste products, and gases. When plasma is frozen and subsequently thawed, a precipitate forms containing a concentrated mix of specific proteins. The liquid that remains after removing this precipitate is called cryopoor plasma.
Why is Cryopoor Plasma Used?
Replacement Therapy for Deficient Proteins:
Some individuals might be deficient in certain proteins that are not part of the cryoprecipitate. In such cases, cryopoor plasma provides a more suitable treatment option.
How Long Does Transfused Blood Stay In The Body?
Blood Components of Blood and Their Lifespan
Before diving into the specific duration of transfused blood in the body, it’s essential to understand that blood isn’t just a homogenous fluid. It is made up of multiple components, each with its own function and lifespan:
Red Blood Cells (RBCs): These are the oxygen-carrying cells. Their primary function is to transport oxygen from the lungs to the body's tissues and take carbon dioxide from the tissues back to the lungs. RBCs have a lifespan of about 120 days. However, not all transfused RBCs last this long, especially since they might not be entirely fresh when transfused.
Platelets: These tiny cell fragments play a critical role in blood clotting. They have a much shorter lifespan than RBCs, typically around 5-7 days. This is one reason platelets are in constant demand in hospitals and blood banks.
White Blood Cells (WBCs): These cells are part of the immune system, defending the body against infections. They have varied lifespans depending on the type of WBC. Some can live for a few hours to a few days, while others, under specific conditions, can last for years. WBCs are typically not transfused and are generally filtered out. Only in very specific instances are White Blood Cells (specifically granulocytes) transfused.
Plasma: This is the liquid component of blood, holding cells, platelets, nutrients, hormones, and waste products. Once transfused, the plasma and its components quickly integrate with the recipient’s own plasma.
Factors Affecting the Lifespan of Transfused Blood
While we've mentioned the typical lifespans of various blood components, it's essential to understand that the actual duration can vary based on several factors:
Age of the Transfused Blood: Blood stored in blood banks is not 'fresh.' RBCs, for example, can be stored for up to 42 days post donation before transfusion. Older blood cells might not function as efficiently and might be removed from circulation sooner than fresher cells. Stored blood undergoes changes over time, a phenomenon known as "storage lesion." As red blood cells age in storage, their flexibility and oxygen-carrying capacity can diminish. Consequently, when transfused, these older cells may be recognized and cleared from the recipient's system faster than newer, more functional cells.
Recipient’s Health: The health status of the blood recipient can influence how long transfused components last in their system. For instance, individuals with bleeding disorders have a heightened tendency to bleed, causing transfused platelets, which aid in clotting, to be utilized more rapidly. Consequently, these patients might require more frequent or larger-volume transfusions to maintain adequate platelet levels.
Compatibility and Immune Response: While blood banks and hospitals ensure compatibility before transfusion, there can still be minor mismatches or reactions, leading to quicker removal of transfused components from the body.
The Journey of Transfused Blood
When transfused blood enters the recipient’s body, it begins its vital work immediately. RBCs start transporting oxygen, platelets assist in clotting, and any transfused WBCs (though they are typically minimized in transfusions) would aid in immune functions.
As these components reach the end of their lifespan, the body has mechanisms to recognize and remove old or damaged cells. The spleen and liver play essential roles in this process. For example, aged or damaged RBCs are identified and broken down in the spleen, with useful components recycled and waste products excreted.
The Lasting Impact of a Blood Transfusion
While the actual cells or platelets from a transfusion might only remain in the body for days to a few months, the impact of a transfusion can be long-lasting. By restoring blood volume, supplying oxygen, or stopping a bleed, transfusions can be the difference between life and death. They give the body the time and resources it needs to heal and recover.
Does a Blood Transfusion Raise Iron Levels?
When a person receives a blood transfusion, they are receiving not only red blood cells but also the iron contained within those cells. Each unit of transfused red blood cells contains about 200-250 mg of iron. The body will break down the transfused red blood cells over time, and the iron from these cells will be released and made available for the body to use or store.
Individuals who often get blood transfusions, like those with chronic diseases or chronic anemia, can end up with too much iron in their bodies. This is termed transfusional iron overload. This overload is concerning because our body can't easily get rid of excess iron. Over time, this iron can accumulate in organs like the heart, liver, and certain glands, which can lead to organ damage.To manage and keep an eye on iron levels in those who get regular transfusions, doctors might:
Check serum ferritin levels: This protein stores iron, and its level can hint at the body's total iron stores. A high ferritin level can mean there's too much iron in the body.
Use iron chelation therapy: This is a treatment where medications are used to bind and remove excess iron from the body. Common medicines for this include deferoxamine, deferasirox, and deferiprone.
Monitor organs: As excess iron can damage organs, it's crucial to keep a regular check on their function. This might include testing liver function or heart evaluations.
Advise on diet: Sometimes, patients might be told to eat less iron-rich food. However, the iron we get from food usually isn't as concerning as the iron from transfusions.
- Phlebotomy: In certain situations, doctors might remove some blood to decrease iron levels. This method is more common for conditions like hereditary hemochromatosis, where the body absorbs too much iron from food.
For certain patients, especially those with sickle cell disease, a specific procedure called Red Blood Cell (RBC) exchange, or erythrocytapheresis, is sometimes recommended. This procedure is different from a simple blood transfusion and can be beneficial in managing iron overload.
Red Blood Cell Exchange for Sickle Cell Patients:
In RBC exchange, the patient's blood is drawn out and passed through a machine that separates the components of the blood. The sickled red blood cells (which are misshapen and can cause blockages in the blood vessels) are removed and replaced with healthy donor red blood cells. The plasma, white blood cells, and platelets are typically returned to the patient. This means that the patient receives fresh red blood cells without a significant increase in blood volume or iron.
Why RBC Exchange Helps with Iron Overload:
Limited Iron Intake: In a standard transfusion, the patient receives additional blood, which brings with it the iron contained in the red blood cells. Over time and with frequent transfusions, this can lead to iron overload. In contrast, with RBC exchange, because the patient's own sickled blood is being removed and replaced, there is no significant net gain in iron.
Chronic Transfusion Alternative: Some sickle cell patients might be on a chronic transfusion regimen to prevent complications like strokes. These regular transfusions can rapidly lead to iron overload. RBC exchange offers a way to get the benefits of the transfusion (like increasing the percentage of healthy red blood cells) without the added risk of iron buildup.
Better Symptom Management: Apart from the iron overload aspect, RBC exchange can also help manage sickle cell crisis symptoms by rapidly decreasing the percentage of sickled cells in circulation.
More About Iron
Iron Homeostasis in the Body: The human body has a sophisticated system for regulating iron levels. The body absorbs iron from food in the intestines and uses it to make hemoglobin in red blood cells. When red blood cells die (typically after about 120 days in circulation), the body recycles the iron. Importantly, humans don't have a direct mechanism to excrete large amounts of iron. So, introducing additional iron via transfusions can disrupt this equilibrium, leading to increased iron stores.Why Iron Overload is Harmful: We touched upon the organ damage caused by iron overload, but it's worth emphasizing that free iron (not bound to proteins) can catalyze the formation of free radicals, which can damage cells, proteins, and DNA. This oxidative stress is what leads to organ damage in conditions like hemochromatosis and transfusional iron overload.
Alternatives to Blood Transfusion: For patients at risk of iron overload, doctors might explore alternatives to blood transfusions when possible. For example:
Erythropoiesis-stimulating agents (ESAs): These are drugs that stimulate the bone marrow to produce more of its own red blood cells, reducing the need for transfusions.
Iron-modifying agents: There are some agents that can bind to free iron in the bloodstream, potentially reducing the risk of iron-related complications.
Optimized surgical and treatment techniques: In surgeries or treatments that might require transfusions, optimizing techniques to minimize blood loss can reduce the need for transfusions.
Individual Variation: Not everyone responds to transfusions in the same way. Some people may absorb and store iron from transfusions more efficiently than others. Factors such as genetics, underlying health conditions, and age can all influence how a person's body handles extra iron.
Iron and Infections: Elevated iron levels and hemochromotosis can increase
susceptibility to certain infections, as many pathogens thrive in
iron-rich environments. This is another reason why managing iron levels
is crucial, especially in patients receiving regular transfusions.
Liquid Plasma
Transfusion medicine continually evolves with the demands of modern healthcare. One key component gaining traction in various clinical scenarios, notably trauma, is liquid plasma. This article delves into the specifics of liquid plasma, its applications, and its significance in today's medical landscape.
What is Liquid Plasma?
Never frozen!

Liquid plasma (LP or LQP) is essentially plasma that has not been frozen after being separated from whole blood or apheresis collections. Unlike fresh frozen plasma (FFP) or thawed plasma, which undergoes freezing and thawing processes, LP is stored at refrigerator temperatures from the time of collection until its expiration.
Why Choose Liquid Plasma?
- Rapid Availability: In emergent situations, especially trauma, the quick availability of LP can be life-saving. There's no need to wait for the thawing process, as with FFP. However LP, is typically used as a 'bridge' so to speak. Patients are given LP until FFP is finished thawing which can often take up to 30 minutes.
- Extended Shelf Life: While FFP needs to be used soon after thawing (5 days max), LP can be stored refrigerated for up to 26 days post-collection.
- Efficacy: LP contains vital clotting factors in amounts similar to FFP, making it effective for coagulopathy reversal.
Applications of Liquid Plasma
- Trauma and Massive Transfusion Protocols (MTP): The immediate availability of LP can be crucial in trauma settings where rapid blood component administration is required, such as a Massive Transfusion Protocol initiation.
- Cardiac Surgery: Some centers use LP for patients undergoing cardiac procedures to manage bleeding complications.
- Liver Disease: LP can assist in clotting factor replacement for patients with liver diseases.
Advantages of Using Liquid Plasma
- Immediate Use: No thawing time ensures rapid administration to patients.
- Reduction in Wastage: The longer shelf life of LP compared to thawed plasma reduces the potential for wastage.
- Safety: LP undergoes the same infectious disease testing as other blood components, ensuring patient safety.
Challenges with Liquid Plasma
- Storage Requirements: To maintain its efficacy, LP requires strict refrigerated storage conditions.
- Limited Availability: Not all blood centers or hospitals stock LP regularly, potentially limiting its widespread use.
- Cost: Producing and storing LP might have associated costs that some institutions find prohibitive.
- Patient Volume: Ensuring that LP is used before expiration really hinges on a busy Transfusion Medicine department. Smaller hospitals would likely not find using Liquid Plasma feasible. Larger hospitals with a dedicated trauma program are more likely to successfully utilize Liquid Plasma.
Looking Ahead
Liquid plasma's role in transfusion medicine is undeniable. Its use in trauma settings underscores its potential to save lives when every second counts. As more clinical evidence emerges supporting its efficacy, it's likely that LP will find even broader applications.
However, as with all medical products, it's essential to weigh the benefits against potential challenges. Proper storage, understanding its indications, and ensuring timely use will determine its place in the medical arsenal.
Liquid plasma offers a promising solution in the rapidly evolving domain of transfusion medicine. Its increasing prominence in trauma care and other clinical situations highlights the need for continued research and understanding of its optimal use.
Neonatal Transfusion
The delicate realm of neonatal transfusions stands distinctively apart from those in adults and older children. The particularities range from why transfusions might be required, the specific volume considerations, to the myriad of potential complications. Let’s navigate this intricate process.
Neonatal Transfusion Indications
Neonates may require transfusions for various reasons:
Prematurity: Infants born prematurely often have a compromised ability to produce red blood cells, necessitating transfusion support.
Hemolytic Disease of the Newborn (HDN): This arises from blood type incompatibility between mother and baby, causing the baby's red blood cells to break down at an accelerated rate.
Surgical Procedures: Major surgeries, such as cardiac interventions, may require transfusions.
Other Conditions: Issues like sepsis, necrotizing enterocolitis (NEC), or specific bleeding disorders can also necessitate a transfusion.
Volume Considerations
Given the limited blood volume of neonates, transfusion requirements are substantially less:
- Packed Red Blood Cells (PRBCs): Typically, 10-15 ml/kg of the infant's weight can increase the hemoglobin level by about 2-3 g/dL.
Blood Types and Compatibility in Neonatal Transfusions
Although type-specific blood would be ideal for any patient, neonatal transfusions have a unique challenge. Due to the possibility of lingering maternal ABO antibodies in the newborn, type-specific blood might lead to complications. Hence, to bypass this risk, blood banks commonly provide O positive or O negative blood for neonates until the close of the neonatal period.
Factors Influencing Blood Quality
Blood Age, 2,3-BPG, and pH Levels: Fresh blood, usually less than 5 days old, is preferable for neonatal transfusions. Fresher blood tends to have higher levels of 2,3-diphosphoglycerate (2,3-BPG) which enhances oxygen release to tissues. Additionally, fresher blood boasts more optimal pH levels, further promoting efficient oxygen transfer to vital organs.
Irradiation: While irradiation is used to prevent graft-versus-host disease (GVHD), it may contribute to increased potassium levels in stored blood. Freshly irradiated (<24 hours post irradiation) is often advised.
Additives and Blood Solutions: Neonatal transfusions preferably use blood with non-additive solutions like CPDA-1. AS-3 is often acceptable as it does not contain mannitol. Blood units containing additives, such as mannitol, are generally avoided because they can pose potential risks for neonates, like volume overload due to the extra additive volume and electrolyte imbalances due to kidney function disruption.
Cytomegalovirus (CMV) Safe Blood: Given their vulnerability, neonates ideally should receive CMV seronegative or leukoreduced blood products to fend off potential CMV infections.
5. Complications to Be Cognizant Of
Hyperkalemia: Due to potassium buildup in stored and irradiated blood, neonates, especially those born prematurely, run the risk of hyperkalemia.
Transfusion-related Acute Lung Injury (TRALI): While uncommon, this can pose a severe threat, emerging from a reaction between donor antibodies and neonatal leukocytes.
Volume Overload: Given neonates' limited cardiovascular endurance, they can easily experience volume overload, potentially leading to heart failure.
6. Monitoring Is Imperative
Continuous Monitoring: It's essential to continuously monitor heart rate, blood pressure, and oxygen saturation levels throughout the transfusion process.
Laboratory Assessments: Pre and post-transfusion, laboratory evaluations like complete blood count, bilirubin, and electrolytes can provide vital information on the transfusion's efficacy and safety.
7. Ethics and Neonatal Transfusions
Considering the intrinsic risks associated with blood transfusions in neonates, these decisions must be approached with caution. Ensuring the parents or guardians are informed and involved in the decision-making process is not just ethical but also integral for trust and transparency.
In essence, neonatal transfusions, while life-saving, necessitate an intricate understanding of the many factors at play. By being informed and cautious, medical professionals can ensure these fragile patients receive the care they critically need during their first days of life.
Why Are There Always Blood Shortages?
The Summer Slump: College Closures and Vacationing Donors
For many, summer evokes images of sun-soaked beaches, barbecues, and long-awaited vacations. However, for blood banks, summer often sounds an alarm. A significant portion of blood donations comes from college and university blood drives. These institutions, with their dense populations of young and often healthy individuals, can be gold mines for blood donations. But once summer starts, campuses empty out, leaving blood banks with a gaping hole in their usual donation numbers.
Furthermore, summer isn’t just a time for students to take a break; it’s the peak travel season. Families, individuals, and even regular donors jet off to vacations, making it less likely for them to donate. While a week-long trip might seem inconsequential, the cumulative effect of many potential donors being away can severely impact blood supplies.
Holidays: A Double-Edged Sword
Holidays, much like summers, are times of joy and relaxation for most. But for blood banks, they can be periods of dread. Holiday weekends see a surge in travel, making potential donors less accessible. Moreover, during festive times, individuals are engrossed in preparations, celebrations, and family gatherings, often placing blood donation low on their priority list. This results in a drop in the blood supply, just when more accidents typically occur due to increased travel, leading to a greater demand for transfusions.
Staffing Struggles in the Blood Donation Realm
Behind every blood donation, there’s an army of professionals ensuring the process runs smoothly. Phlebotomists, the trained professionals who draw blood, are the frontline soldiers in this battle against shortages. Their expertise ensures that blood is drawn safely, efficiently, and with minimal discomfort to the donor.
However, like many specialized professions, there’s a shortage of skilled phlebotomists. The reasons are manifold. Phlebotomy, despite its importance, may not offer competitive remuneration in all regions or institutions. The job, being hands-on and requiring impeccable precision, can be high-pressure. Mistakes are not an option, leading to a steep learning curve and rigorous training requirements.
Then there are the couriers, the vital links that ensure donated blood reaches its destination promptly. These individuals often work irregular hours, handling delicate packages that can mean life or death for someone. The demand for timely transportation of blood can be especially high during emergencies or natural disasters.
Drive workers, the people who set up and manage the infrastructure for blood drives, also face unique challenges. Organizing a drive requires meticulous planning, coordination with multiple agencies, and the ability to manage large groups of donors. Finding individuals skilled in such tasks, willing to work on a schedule dictated by the community’s needs, can be daunting.
Operational Hiccups and Challenges
Maintaining a consistent blood supply isn't just about getting donors in the door. It's a complex ballet of logistics, where blood collected needs to be tested, processed, stored, and then dispatched as required. Each of these stages requires specialized staff, equipment, and facilities. Even minor disruptions, be it equipment malfunctions or delays in transportation, can cause bottlenecks. With blood having a limited shelf life – 42 days for red blood cells and just five days for platelets – these delays can result in wastage, further exacerbating shortages.
Public Perceptions and Myths
Misconceptions surrounding blood donations can also play a role in shortages. Fears about pain, side effects, or contracting diseases deter potential donors. While awareness campaigns are working to combat these myths, they persist in sections of the community, creating barriers to donation.
Pandemics and Health Crises
Global health crises, such as the COVID-19 pandemic, pose unprecedented challenges for blood banks. The fear of getting infected deters many potential donors from visiting donation centers. Moreover, lockdowns and social distancing measures further limit the ability to conduct large-scale donation drives. During the initial stages of the pandemic, many blood drives were canceled, causing an immediate and concerning drop in available blood supplies.
The Financial Dynamics
Blood donation, at its heart, is a philanthropic act, but the operations surrounding it are undoubtedly bound by financial constraints. Blood banks have to balance between operational costs, testing, storage, and transportation. Profit margins can be slim, especially for non-profit blood centers. The economics becomes even more challenging when there's a need for rare blood types or specialized blood products, which might cost more to process but are essential for specific patient populations.
Generational Shifts in Attitudes
While it's a broad generalization to say newer generations don’t recognize the importance of donating blood, there has been a noted shift in outreach methods needed to engage them. Traditional awareness campaigns might not resonate as much with younger generations, necessitating a shift to digital platforms, influencers, and other modern outreach strategies. If these shifts aren't made promptly or effectively, it can lead to decreased engagement from younger potential donors.
Educational Gaps
Over the years, there has been a fluctuation in emphasis on community service and civic duties in educational curriculums. While some schools and colleges have robust programs encouraging blood donation, others might lack such initiatives. A consistent, nationwide (or even global) emphasis on the importance of blood donation in educational settings could help instill the habit in individuals from a young age.
Commercialization and Profit Motives
Some blood banks operate on a for-profit model, leading to concerns about the commercialization of what many see as a purely altruistic act. This commercial angle can sometimes deter potential donors who might feel uneasy about their donation becoming a commercial product. It's a delicate balance for these institutions to maintain operational efficiency while ensuring the trust of the donor community.
Regional Disasters and Traumas Impacting Blood Supplies
Every region, whether it's due to its geographical location, climate, or other factors, is vulnerable to specific types of disasters. For instance, coastal areas might face hurricanes, while tectonically active zones could be at risk of earthquakes. When these disasters strike, the medical needs of the affected populace surge dramatically, including a sudden increase in demand for blood.
Natural disasters often result in injuries that require surgical interventions, thereby increasing the demand for blood products. Similarly, large-scale accidents or mass trauma incidents, like major vehicle pile-ups or industrial accidents, can exert sudden pressure on available blood supplies.
Concurrently, these disasters can disrupt regular blood donation activities. Blood banks in the affected areas might be damaged, or transportation routes could be blocked, preventing the timely arrival of much-needed blood from other regions. Also, regular donors might be affected by the disaster themselves, making them temporarily unavailable to contribute.
Moreover, even if a region isn't directly affected by a disaster, it might be called upon to support a neighboring area that is. This can strain local supplies, especially if there's already an existing shortage.
Understanding the dual challenge posed by increased demand and potential disruptions during disasters underscores the need for robust contingency plans. Blood banks, in collaboration with local and national agencies, must be prepared to rapidly scale up their operations and ensure that they can meet the sudden surge in demand while also navigating the logistical challenges posed by the disaster.
What now?
The persistent problem of blood shortages, at its core, is a multi-faceted challenge. It intertwines with societal behaviors, professional shortages, operational challenges, and public perceptions. Addressing it requires not just rallying more donors but also creating robust systems that can efficiently handle donations, fostering professional growth in the industry, and constantly battling misconceptions with information. As our understanding of these intricacies grows, so does our hope for a future where blood shortages become a relic of the past.
Bombay Phenotype
What is Bombay phenotype?
The Bombay phenotype is a rare blood type that occurs when an individual has inherited two copies of a recessive gene that affects the production of certain antigens on the surface of red blood cells. Specifically, individuals with Bombay phenotype do not produce the H antigen, which is the precursor to the A and B antigens that determine the ABO blood type system. As a result, people with Bombay phenotype have blood that appears to be type O, even though they may have genes for type A or B blood.
How does Bombay phenotype affect transfusions?
Because people with Bombay phenotype lack the H antigen, their blood can be incompatible with blood from other ABO blood types. This means that people with Bombay phenotype cannot receive blood from most other blood types, including type A, B, AB, and O. In fact, people with Bombay phenotype can only receive blood from other individuals with the same rare blood type.
For this reason, it is essential that individuals with Bombay phenotype are identified and properly tested before any blood transfusions. If someone with Bombay phenotype receives blood from an incompatible blood type, it can lead to a severe and potentially life-threatening reaction known as a transfusion reaction.
What steps can be taken to ensure safe transfusions for people with Bombay phenotype?
To ensure the safety of people with Bombay phenotype who require blood transfusions, it is crucial to identify individuals with this rare blood type early on. This can be done through blood typing tests, which can determine whether or not someone has the H antigen.
Once someone with Bombay phenotype has been identified, steps can be taken to ensure that they receive compatible blood during transfusions. This typically involves identifying other individuals with the same rare blood type and maintaining a supply of their blood for use in transfusions. Blood banks and hospitals often work together to create networks of donors with rare blood types, including Bombay phenotype, to ensure that there is always a supply of compatible blood available.
In addition to proper identification and blood banking, it is also important to monitor people with Bombay phenotype closely during and after blood transfusions. This can help to identify any potential complications or adverse reactions early on and ensure that prompt treatment is provided if necessary.
Frozen Blood
Blood for people with Bombay phenotype can be frozen and stored for future use, and one of the most common methods of blood preservation is glycerolization.
Glycerolization is a process in which red blood cells are mixed with a solution of glycerol and other chemicals before freezing. This solution helps to protect the cells from damage during the freezing and thawing process and allows the blood to be stored for longer periods of time.
During glycerolization, the red blood cells are mixed with a solution containing glycerol, a sugar called trehalose, and other chemicals that help to stabilize the cells. The cells are then slowly cooled to a temperature below freezing, typically around -80°C. Once the cells are frozen, they can be stored for several years, if necessary, without significant loss of quality.
When the blood is needed for transfusion, the frozen blood is thawed slowly and carefully, and the glycerol and other chemicals are removed. The red blood cells can then be transfused into the patient as needed.
Glycerolization is a common method of blood preservation for people with rare blood types like Bombay phenotype because it allows compatible blood to be stored for longer periods of time, which can be especially important in emergency situations or when a suitable donor is not immediately available.
Autologous Donation
People with Bombay phenotype can donate their own blood for autologous transfusions. In fact, autologous blood donation can be a valuable strategy for people with rare blood types like Bombay phenotype to ensure that they have access to compatible blood when needed.
Autologous blood donation involves collecting and storing a person's own blood for future transfusion. The process usually involves donating blood several weeks or months before it is needed, and the blood is tested and processed to ensure that it is safe and compatible with the person's own blood type.
Because people with Bombay phenotype have a rare blood type that is not compatible with most other blood types, autologous blood donation can be a useful strategy for ensuring that they have access to compatible blood when needed. It can be particularly important in situations where there may be limited access to compatible blood, such as in remote or resource-limited settings.
It's important to note that the process of autologous blood donation and transfusion requires careful planning and coordination to ensure that the blood is collected, processed, and stored properly, and that it is used before it reaches its expiration date.
Blood Donor Eligibility Requirements
Blood Donation Requirements
 |
| Blood donation is one of the most important and selfless things you can do to save a life! |
The blood donor requirements in the US may vary slightly depending on the blood center or blood bank, but in general, donors must meet the following criteria:
- Age: Donors must be at least 17 years old (16 years old with parental consent in some states).
- Weight: Donors must weigh at least 110 pounds.
- Health: Donors must be in good health, feeling well, and free from cold or flu symptoms.
- Hemoglobin level: Donors must have a hemoglobin level of at least 12.5 grams per deciliter (g/dL) for females and 13.0 g/dL for males.
- Medications: Some medications can affect eligibility, so donors should inform the blood center staff of any medications they are taking.
- Travel and residency: Donors who have traveled to certain countries or lived in certain regions may be deferred for a period of time due to potential exposure to infectious diseases.
- Sexual activity: Donors who engage in certain high-risk sexual activities or have been diagnosed with certain sexually transmitted infections may be deferred.
- Medical history: Donors with certain medical conditions or histories may be deferred, such as those with a history of cancer or certain heart conditions.
It's important to note that these requirements are in place to ensure the safety of both the donor and the recipient of the blood donation. Potential donors should contact their local blood center or blood bank to confirm their eligibility to donate, such as their local Red Cross, Bloodworks Northwest, Vitalant, etc.
Common Blood Donation Deferrals:
Recent illness: If you have had a fever or an illness, you may be deferred from donating blood until you have fully recovered.
Recent travel: If you have recently traveled to certain countries or regions, you may be deferred from donating blood due to the risk of exposure to infectious diseases such as malaria, Zika virus, or Ebola.
Anemia: If you have a low hemoglobin level or are anemic, you may be deferred from donating blood.
Medications: Certain medications may defer someone from donating blood, such as blood thinners, aspirin, or certain antibiotics.
High-risk behavior: If you engage in certain high-risk behaviors, such as using intravenous drugs or having unprotected sex, you may be deferred from donating blood due to the risk of transmitting infections such as HIV, hepatitis B or C, or syphilis.
There are several diseases and conditions that may defer someone from donating blood in the US. Some of the common ones include:
- HIV or AIDS
- Hepatitis B or C
- Syphilis
- Malaria
- Creutzfeldt-Jakob Disease (CJD) or Variant Creutzfeldt-Jakob Disease (vCJD)
- Zika virus infection
- Babesiosis
- Chagas disease
- West Nile virus infection
- Ebola virus infection
In addition to these diseases, some medical conditions may also defer a person from donating blood, such as certain types of cancer, heart disease, and autoimmune disorders.
Can you donate blood if you have tattoos?
Yes, you can donate blood if you have a tattoo in most cases, but the eligibility criteria may vary depending on the tattoo's age and the state where the donation takes place.
In general, if you have had a tattoo, piercing, or any other form of body art, you may be temporarily deferred from donating blood for a certain period. The deferral period is usually 3-12 months, depending on the state and the type of tattoo or piercing. This is because there is a risk of infection from the needles and ink used in the tattoo process.
However, if the tattoo was done in a state-regulated and licensed facility, and if the tattoo artist used sterile needles and ink, the deferral period may be shorter or even waived.
Can I Donate Blood If I Have Cancer?
In general, individuals who have been diagnosed with cancer are typically deferred from donating blood in the US, as there is a risk of transmitting cancer cells through blood transfusions. However, there may be some exceptions depending on the type of cancer and the stage of the disease.
If you have been diagnosed with cancer, you should consult with your doctor to determine your eligibility to donate blood. Your doctor can provide specific guidance on whether or not you are eligible to donate blood based on your individual medical history and current health status.
In some cases, individuals who have had certain types of cancer and have been cancer-free for a certain period of time may be eligible to donate blood. However, this may vary depending on the blood center or blood bank and the specific criteria they have in place.
The specific types of cancer that may prevent someone from donating blood include:
- Leukemia or lymphoma: These are cancers that affect the blood and bone marrow and may increase the risk of transmission of cancer cells through blood transfusions.
- Multiple myeloma: This is a type of cancer that affects plasma cells, which may also increase the risk of cancer cell transmission through blood transfusions.
- Hodgkin's disease: This is a type of lymphoma that affects the lymphatic system and may also increase the risk of cancer cell transmission through blood transfusions.
- Other types of cancers: Individuals who have been diagnosed with other types of cancers may also be deferred from donating blood, depending on the type and stage of the cancer.