What are Washed Blood Products?
Washing blood products is necessary in certain populations who may have certain adverse reactions to receiving blood components.
Washing blood products involves mixing the product with a neutral solution, most commonly 0.9% Normal Saline. The product is then centrifuged to separate the cellular and liquid portion. The liquid portion is then removed from the bag. This process is typically performed multiple times in a row to ensure the removal of unwanted solutes.
Washing can be done manually using a Blood Bag centrifuge, or the process can be done (mostly) automatically using a Blood Cell Washer designed specifically to wash blood products. This washing process helps to remove plasma proteins (including antibodies) as well as excess electrolytes that may be present in the bag. Only Red Blood Cell and Platelet units are washed. Plasma/FFP units CAN NOT be washed. The washing process is designed to REMOVE plasma, thus would prove counterintuitive.
Washing can be done manually using a Blood Bag centrifuge, or the process can be done (mostly) automatically using a Blood Cell Washer designed specifically to wash blood products. This washing process helps to remove plasma proteins (including antibodies) as well as excess electrolytes that may be present in the bag. Only Red Blood Cell and Platelet units are washed. Plasma/FFP units CAN NOT be washed. The washing process is designed to REMOVE plasma, thus would prove counterintuitive.
 |
| The front face of a Terumo COBE 2991 Automated Cell Processor used in washing blood products |
The centrifuge bowl of an automatic cell washer. A specialized circular "donut" shaped blood bag is used to fit inside of the machine. Blood may be kept within this bag after washing and transfused as such, or it can be transferred to a normal 300 or 600mL blood bag.
Who Needs Washed Blood Components?
Patients who have previously had severe allergic reactions to receiving blood components should likely be transfused washed blood products. They may be allergic to constituents of the additive solutions, leftover anticoagulants in the bag, or plasma proteins in the small amount of plasma that may be left in the unit.
IgA Deficiency or Anti-IgA
Patients who have a true IgA deficiency or HAVE made Anti-IgA, an antibody directed towards IgA, should receive washed blood products as the plasma from a normal healthy donor would contain small amounts of IgA. IgA is a type of antibody present in small amounts in normal healthy individuals. IgA deficiency is often the result of a genetic mutation. There are acquired, non-genetic, factors leading to a transient IgA deficiency as well.
A patient with a true IgA deficiency is at risk of creating an anti-IgA antibody. If transfused with unwashed blood, this anti-IgA may react with the IgA that may be present in the donor blood product. This can potentially cause severe anaphylactic transfusion reactions.
Patients with Anti-IgA who may need plasma/FFP for any reason should receive IgA deficient plasma.
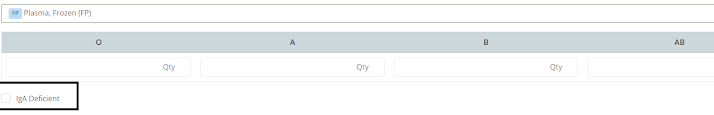 |
| Blood Centers utilizing the online blood ordering system BloodHub make it easy to request IgA deficient plasma. |
Hyperkalemia
Hyperkalemia refers to an elevated potassium level within the blood. Patients who have or are at risk of hyperkalemia can receive washed Red Blood Cell units. The act of washing can remove most of the excess potassium from the unit.
As a unit of blood ages, the Red Blood Cells start to lose their ability to keep potassium within their cells and potassium begins to leak out of the cells into the liquid portion of the unit adding to what is called the "storage lesion". The storage lesion include all of the changes the unit of Red Blood Cells go through as it ages (increased potassium, decreased glucose, decreased ATP, etc). This potassium leakage effect can actually be exacerbated by irradiating the Red Blood Cells. For normal healthy individuals, the amount of potassium in the unit being transfused is acceptable and well tolerated by the vast majority of individuals.
Platelets do not generally get washed for hyperkalemia indications, as they do not leech potassium like a Red Blood Cell unit might.
Patients with with severe kidney disease may require washed Red Blood Cells if they are unable to maintain a normal potassium level. Even patient's receiving regular dialysis will often have washed cells ordered simply as a precaution to mitigate any potential for hyperkalemic events.
Depending on the transfusion center, fresh units of Red Blood Cells may be substituted for washed units in hyperkalemic scenarios. A fresh unit, one that was collected within five to seven days, is unlikely to have built up enough potassium in the bag to affect the patient. This is the ordering physician's call.
Deglycerolizing Frozen RBC Units
Another reason for washing would be to remove the glycerol added to frozen Red Blood Cell units once they are thawed. Blood that is collected from donors that have extremely rare blood phenotypes may be frozen so that it is available if a patient comes along who may need it. Glycerol must be added to the unit of Red Blood Cells before freezing, or the Red Cells would pop or "lyse" during the freezing process. Glycerol helps to prevent this from happening. Once thawed, the glycerol needs to be removed prior to transfusion. Washing of the Red Blood Cells is a common way to ensure the glycerol has been safely removed.
Neonates and ECMO
Some transfusion centers will have procedures for washing products for specific purposes in neonatal populations. It is not common to wash Red Blood Cells for simple small volume transfusions for neonates. Some facilities may choose to wash Red Cell units used for the priming of an ECMO circuit for any neonate being out on ECMO.
ECMO is Extracorporeal Membrane Oxygenation, which is a machine that will oxygenate the blood outside of the body for a patient when they are unable to adequately do so themselves. This large volume of blood being fed into a machine that can potentially causes hemolysis (destruction of the cells) could benefit from being washed to reduce the amount of transfused potassium, averting a hyperkalemic event. Additionally it spares the neonate from coming in contact with a larger amount of plasma proteins, etc., that may be in the unit.
ECMO is Extracorporeal Membrane Oxygenation, which is a machine that will oxygenate the blood outside of the body for a patient when they are unable to adequately do so themselves. This large volume of blood being fed into a machine that can potentially causes hemolysis (destruction of the cells) could benefit from being washed to reduce the amount of transfused potassium, averting a hyperkalemic event. Additionally it spares the neonate from coming in contact with a larger amount of plasma proteins, etc., that may be in the unit.
Another uncommon washing tactic involves a rare but serious disease known as Fetomaternal alloimmune thrombocytopenia, where a mother makes an antibody towards antigens on the baby's platelets. If the the neonate were to need a platelet transfusion, it would be important to choose platelets that are negative for the platelet antigen that the mother has made an antibody towards.
The easiest choice in donor in this case would oddly enough be the mother. If she made an antibody, it can be assumed she is negative for the antigen, and her immune system created an antibody as a result of seeing something 'foreign'. The donated platelets should then be washed multiple times to ensure the maternal platelet antibody is removed from the unit so that it would not attack more of the neonate's platelets once transfused.
The easiest choice in donor in this case would oddly enough be the mother. If she made an antibody, it can be assumed she is negative for the antigen, and her immune system created an antibody as a result of seeing something 'foreign'. The donated platelets should then be washed multiple times to ensure the maternal platelet antibody is removed from the unit so that it would not attack more of the neonate's platelets once transfused.
Cons to Washing Blood Products
- Recovery yields of a product are generally lower than the original product. It is nearly impossible to retain 100% of the product while washing, and some of the product will be lost during the washing steps. Platelets could be lost up to 30% of the original yield. Up to 20% of Red Blood Cells can be lost to washing. Thus, a single unit of these products may not increase a patient's counts as expected. It is expected to see a decreased Corrected Count Increment for washed platelets.
- Washed platelets expire four hours after washing. Washed Red Blood Cells expire 24 hours after washing. It is imperative that this is communicated to the clinical team so that the products actually get used and not wasted due to their shortened outdates.
- Washed products cannot be given upon an emergent request. Using an automated cell washer can still require up to 30 minutes to wash and process a single Red Cell Unit and even longer for platelets.
